sliding scale insulin pdf
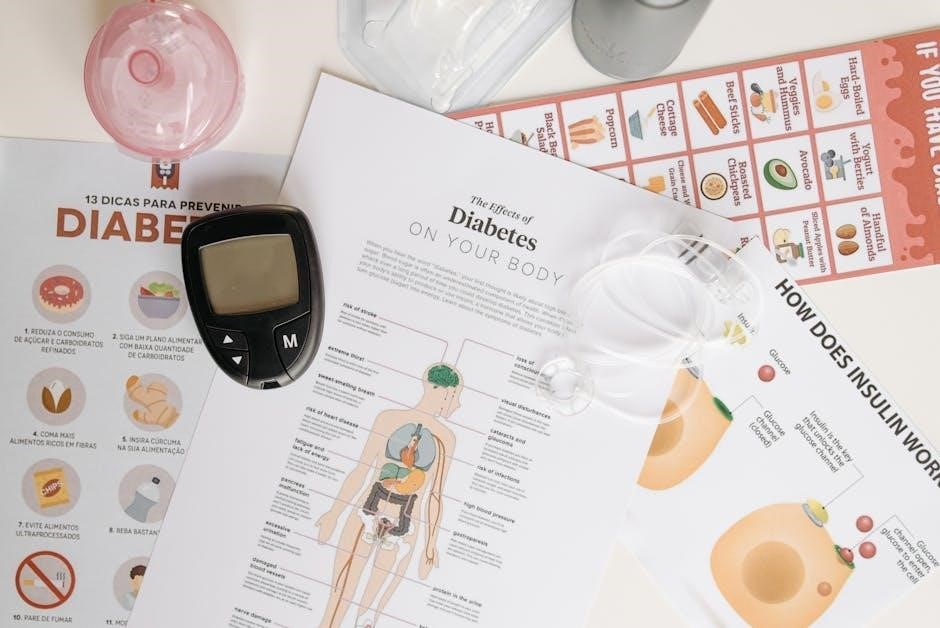
Understanding Sliding Scale Insulin
Sliding scale insulin protocols, often documented in PDF formats, adjust dosage based on blood glucose levels; however, current guidelines recommend avoiding sole reliance on this method.
Practical guides to insulin therapy, like the 2024 edition, emphasize comprehensive diabetes management, and sliding scale protocols are frequently included as examples.
Sample protocols, available as PDFs, detail dosage adjustments—for instance, a medium-dose scale might prescribe 2-4 units based on glucose ranges of 120-200 mg/dL.
What is Sliding Scale Insulin?
Sliding scale insulin is a method of administering insulin where the dosage is adjusted based on a patient’s current blood glucose level. Often detailed in hospital protocols available as PDF documents, it involves pre-defined ranges and corresponding insulin unit amounts.
These PDF guides typically present a table outlining glucose ranges – for example, below 70 mg/dL triggers hypoglycemia treatment, while levels between 120-150 mg/dL might warrant a 2-unit dose. The intention is to correct hyperglycemia, but it’s frequently used reactively rather than proactively.
However, contemporary guidelines, such as those from the American Diabetes Association and PALTmed, increasingly discourage its use as a sole treatment strategy. PDF resources often include disclaimers emphasizing this point, advocating for basal-bolus regimens or continuous insulin infusion instead. It’s a reactive approach, not a long-term solution.
Historical Context of Sliding Scale Insulin Use
Historically, sliding scale insulin emerged as a pragmatic solution before the advent of more sophisticated diabetes management techniques. Early hospital protocols, often documented in PDF format, relied heavily on this reactive approach to hyperglycemia. These PDFs showcase a time when frequent blood glucose monitoring wasn’t readily available.
The method gained prominence due to its perceived simplicity, allowing nurses to adjust insulin doses without direct physician orders for every change. However, as understanding of diabetes evolved, the limitations of solely relying on sliding scale became apparent.
Modern guidelines, reflected in updated PDF resources from organizations like the ADA, now emphasize proactive basal-bolus regimens. The historical reliance on sliding scale is now viewed as a less effective, and potentially dangerous, practice, often leading to inconsistent glucose control.
The Controversy Surrounding Sliding Scale Insulin
The ongoing debate surrounding sliding scale insulin, often detailed in critical analyses available as PDFs, centers on its reactive nature and potential for inconsistent glucose management. Numerous professional organizations, including those issuing “Choosing Wisely” recommendations, advise against its use as a standalone therapy.
PDF reports highlight the risk of hypoglycemia, particularly when sliding scale is employed without adequate basal insulin coverage. This reactive approach fails to address underlying insulin deficiencies or resistance.
Furthermore, retrospective evaluations, documented in research PDFs, demonstrate that sliding scale algorithms don’t consistently prevent severe hyperglycemia. The controversy stems from its perceived convenience versus its demonstrably suboptimal clinical outcomes, prompting a shift towards more proactive strategies.
Components of a Sliding Scale Insulin Protocol
Sliding scale insulin PDFs outline blood glucose ranges, corresponding insulin dosages, and the type of insulin used—typically rapid-acting or regular—for adjustments.
These protocols detail specific insulin units based on glucose levels, ensuring clear instructions for healthcare professionals administering the treatment.
Blood Glucose Level Ranges
Sliding scale insulin PDFs meticulously define blood glucose ranges, forming the foundation of dosage adjustments. These ranges are typically categorized to guide insulin administration, often starting with levels indicating hypoglycemia (below 70 mg/dL), requiring immediate intervention per nursing protocols.
Common ranges then progress through normal levels (71-119 mg/dL), where no additional insulin is administered, followed by moderate hyperglycemia (120-150 mg/dL), potentially triggering a 2-unit dose, and higher ranges (151-200 mg/dL) warranting 4 units or more.
Protocols may extend to even higher glucose levels, with corresponding increased insulin dosages. The specific ranges and dosages vary between institutions and individual patient needs, but the PDF clearly outlines these parameters for consistent application.
These defined ranges are crucial for safe and effective glucose management.
Insulin Dosage Adjustments
Sliding scale insulin PDFs detail precise insulin dosage adjustments correlated with defined blood glucose ranges. These adjustments are the core of the protocol, dictating how much insulin to administer based on the patient’s current glucose level.
For example, a typical scale might prescribe no insulin for levels between 71-119 mg/dL, 2 units for 120-150 mg/dL, and 4 units for 151-200 mg/dL. Higher ranges necessitate larger doses, carefully outlined in the PDF.
The PDF emphasizes that these are supplemental doses, often alongside a basal insulin regimen. Adjustments are made before meals or at bedtime, as specified in the protocol. Consistent application of these dosage adjustments, as detailed in the PDF, is vital for effective glucose control.
Careful monitoring is essential after each adjustment.
Types of Insulin Used in Sliding Scales
Sliding scale insulin PDFs commonly feature either rapid-acting or regular insulin, detailing their specific applications within the protocol. Rapid-acting insulin (Lispro, Aspart, Glulisine) is favored for its quicker onset, aligning well with mealtime coverage.
However, regular insulin remains a viable option, particularly in hospital settings, and is frequently documented in older PDF protocols. The PDF will specify the precise type used and its corresponding action profile.
When utilizing regular insulin, the PDF must clearly indicate the timing of administration—typically 30-60 minutes before meals—to account for its slower onset. Newer PDFs may highlight the benefits of rapid-acting analogs for improved glucose control.
The choice impacts the overall effectiveness of the scale.
Rapid-Acting Insulin (Lispro, Aspart, Glulisine)
Sliding scale insulin PDFs increasingly favor rapid-acting insulin analogs—Lispro, Aspart, and Glulisine—due to their pharmacokinetic profiles. These PDFs will detail their faster onset (15-30 minutes) and shorter duration of action, offering more precise glucose correction.
The PDF documentation emphasizes administering these insulins immediately before or within 15 minutes of meal initiation, crucial for effective coverage. Dosage charts within the PDF are tailored to the rapid action, often requiring smaller units.
Compared to regular insulin PDFs, these protocols require more frequent blood glucose monitoring to prevent hypoglycemia, a point clearly outlined in the documentation.
The PDF will also specify storage guidelines for optimal potency.
Regular Insulin
Sliding scale insulin PDFs historically utilized regular insulin, though its use is now often superseded by rapid-acting analogs. These PDF documents will specify a slower onset of action (30-60 minutes) and a longer duration (5-8 hours) compared to newer options.
PDF protocols using regular insulin necessitate administration 30-60 minutes before meals, a critical timing detail emphasized within the documentation; Dosage charts in these PDFs typically involve larger unit adjustments;
Due to its prolonged action, PDFs highlight the increased risk of delayed-onset hypoglycemia, requiring careful monitoring and patient education.
Recent research, as reflected in some PDF updates, evaluates algorithms using regular insulin to identify patients at risk for severe hyperglycemia.

Creating a Sliding Scale Insulin PDF
Sliding scale insulin PDFs require essential information, clear formatting, and legal disclaimers; sample protocols are often included for practical application and reference.
These PDFs must detail glucose ranges, insulin dosages, and monitoring frequency, ensuring usability for healthcare professionals and patients alike.
Essential Information to Include
A comprehensive sliding scale insulin PDF must contain critical elements for safe and effective implementation. Firstly, clearly define blood glucose level ranges corresponding to specific insulin dosage adjustments. Include a detailed table outlining these ranges and associated unit amounts. Secondly, specify the type of insulin used – rapid-acting or regular – and its onset, peak, and duration of action.
Furthermore, the PDF should explicitly state the frequency of blood glucose monitoring, such as before meals and at bedtime, and instructions for “as needed” checks. Detail hypoglycemia and hyperglycemia management protocols alongside the sliding scale. Patient-specific information, like allergies and other medications, should be noted. Finally, a clear disclaimer stating the protocol is a guide and requires physician oversight is crucial for legal protection and responsible care.
Formatting for Clarity and Usability

When creating a sliding scale insulin PDF, prioritize clear and concise formatting. Utilize a tabular layout for the blood glucose ranges and corresponding insulin dosages, enhancing readability. Employ bold text for key headings and values. Consistent font styles and sizes are essential for a professional appearance.
Incorporate ample white space to prevent visual clutter. Consider color-coding to differentiate dosage levels or highlight critical information. Ensure the PDF is easily printable and accessible on various devices. Include a prominent section for notes, allowing healthcare professionals to document individual patient adjustments. A well-organized PDF minimizes errors and promotes efficient workflow, ultimately improving patient safety and care.
Legal and Disclaimer Considerations
A sliding scale insulin PDF must include a comprehensive disclaimer stating it’s a guideline, not a substitute for professional medical judgment. Clearly indicate the document is intended for qualified healthcare professionals only. Specify the date of creation and any revision history to ensure users have the most current information.
Address potential liability by stating the institution or author isn’t responsible for adverse events resulting from improper use. Include a statement emphasizing the importance of individualized patient assessment and monitoring. Reference relevant guidelines, such as those from the ADA, to demonstrate adherence to standards of care. Consult legal counsel to ensure compliance with all applicable regulations and protect against potential claims.

Sliding Scale Insulin Protocols: Examples
Sliding scale insulin PDFs often present protocols for mild to severe hyperglycemia, alongside hypoglycemia management; sample protocols detail specific dosage adjustments.
A medium-dose example within a PDF might prescribe 2-4 units for glucose levels between 120-200 mg/dL, illustrating typical protocol structures.
Mild to Moderate Hyperglycemia Protocol
Sliding scale insulin PDFs frequently detail protocols for managing mild to moderate hyperglycemia, typically defined as blood glucose levels between 140-250 mg/dL. These protocols outline specific rapid-acting insulin dosage adjustments based on pre-meal glucose readings.
For example, a common protocol, often found within these PDF documents, might suggest no additional insulin for levels 140-179 mg/dL, 2 units for 180-219 mg/dL, and 4 units for 220-250 mg/dL. It’s crucial to remember these are examples, and individual protocols vary.
These PDFs emphasize the importance of rechecking blood glucose levels after insulin administration to ensure effectiveness and prevent hypoglycemia. Furthermore, they often include instructions to notify a physician if glucose levels remain consistently elevated despite dosage adjustments.
Consistent monitoring and documentation, as highlighted in these resources, are vital for effective hyperglycemia management.
Severe Hyperglycemia Protocol

Sliding scale insulin PDFs addressing severe hyperglycemia (generally >250 mg/dL) emphasize a shift from solely relying on the scale to more aggressive interventions. These protocols often indicate contacting a physician immediately for orders beyond the standard sliding scale adjustments.
PDF documents may outline temporary increases in insulin dosage, potentially utilizing correction doses of rapid-acting insulin in addition to the scheduled dose, but always under medical direction. Frequent blood glucose monitoring – every 2-4 hours – is paramount.
These resources stress the need to rule out underlying causes like infection or medication non-adherence. Intravenous fluids may be ordered to address dehydration, a common consequence of high glucose.
PDFs will typically not provide specific dosage recommendations for severe cases, instead prioritizing physician involvement and a comprehensive assessment.
Hypoglycemia Management Alongside Sliding Scale
Sliding scale insulin PDFs invariably dedicate sections to hypoglycemia management, recognizing it as a significant risk with this approach. Protocols emphasize immediate treatment of blood glucose levels below 70 mg/dL with 15-20 grams of rapid-acting carbohydrates – juice, glucose tablets, or regular soda.
PDF documents detail rechecking blood glucose after 15 minutes; if still low, repeating the carbohydrate administration. Once above 70 mg/dL, a snack containing both carbohydrates and protein is recommended to prevent recurrence.
Crucially, these PDFs instruct nurses to investigate the cause of hypoglycemia, adjusting the sliding scale or basal insulin as needed, with physician approval.
Severe hypoglycemia (loss of consciousness or seizure) requires glucagon administration, as outlined in hospital policy, detailed within the PDF.

Alternatives to Sliding Scale Insulin
Sliding scale insulin PDFs often acknowledge superior alternatives like basal-bolus regimens and insulin pumps for consistent glucose control, promoting better outcomes.
Oral hypoglycemic agents are also presented as viable options, depending on the patient’s specific diabetes type and overall health status.
Basal-Bolus Insulin Regimen
Basal-bolus insulin represents a significant departure from the reactive approach of sliding scale insulin, often detailed in comparative PDF resources. This regimen mimics the body’s natural insulin secretion, utilizing a long-acting insulin (basal) to provide a steady background level and rapid-acting insulin (bolus) to cover meals and correct high glucose readings;
Unlike sliding scale, which adjusts doses solely based on current blood sugar, basal-bolus therapy involves proactive dose adjustments based on carbohydrate intake, activity levels, and prior glucose trends. Many PDF guides highlight the benefits of this method, including improved glycemic control and reduced risk of hypoglycemia.
Furthermore, the adoption of second-generation basal insulins like glargine-300 and degludec, discussed in recent research, can further refine the basal component, offering a more predictable and consistent effect. This proactive strategy, detailed in educational PDFs, is generally favored over reactive sliding scales.
Continuous Subcutaneous Insulin Infusion (CSII) ⏤ Insulin Pumps
Continuous Subcutaneous Insulin Infusion (CSII), commonly known as insulin pump therapy, offers a sophisticated alternative to both sliding scale insulin and traditional basal-bolus regimens, often explained in detailed PDF guides; These pumps deliver a continuous, customizable basal rate of insulin, alongside bolus doses for meals, providing a more precise insulin delivery system.
Hospital policies regarding pump use during hospitalization are frequently outlined in PDF protocols, emphasizing the importance of patient education and staff familiarity with the device. CSII allows for greater flexibility and personalization, potentially improving glycemic control compared to sliding scale approaches.
Furthermore, integration with Continuous Glucose Monitoring (CGM) systems, often detailed in comprehensive PDF resources, enables automated insulin adjustments and alerts, minimizing the need for reactive sliding scale corrections and enhancing overall diabetes management.
Oral Hypoglycemic Agents
Oral hypoglycemic agents represent another viable alternative to sliding scale insulin, particularly for patients with Type 2 diabetes, and their use is often detailed within comprehensive diabetes management PDFs. These medications work by improving the body’s insulin sensitivity or increasing insulin production, helping to lower blood glucose levels.
Unlike sliding scale, which reacts to existing hyperglycemia, oral agents aim to proactively manage glucose control. Treatment algorithms, frequently presented in PDF format, guide clinicians in selecting the most appropriate agent or combination of agents based on individual patient characteristics.
While not a direct replacement in all scenarios, incorporating oral medications can reduce or even eliminate the need for sliding scale insulin, promoting more stable and predictable glycemic control, as highlighted in various clinical practice PDF guidelines.

Guidelines and Recommendations (2024-2026)
Guidelines from ADA and PALTmed, often found in PDFs, consistently recommend avoiding sliding scale insulin as a sole treatment strategy for hyperglycemia.
PDF resources detail the need for individualized plans, and emphasize comprehensive diabetes care over reactive sliding scale adjustments.
American Diabetes Association (ADA) Standards of Care
The American Diabetes Association (ADA) Standards of Care, frequently accessible as comprehensive PDF documents, strongly discourage the routine use of sliding scale insulin as the primary method for managing hyperglycemia in hospitalized patients.
These standards emphasize a shift towards more proactive and individualized basal-bolus insulin regimens, promoting tighter glucose control and minimizing the risks associated with reactive sliding scales.
PDF publications from the ADA highlight that sliding scale insulin alone often leads to inconsistent glucose levels, increased risk of hypoglycemia, and doesn’t address the underlying causes of hyperglycemia.
The ADA recommends that hospitals develop and implement policies that prioritize scheduled insulin administration, alongside glucose monitoring, and only utilize sliding scale as a supplemental tool when needed, not as a standalone treatment.
These guidelines are regularly updated and available for download in PDF format on the ADA’s official website, providing healthcare professionals with the latest evidence-based recommendations.
PALTmed Guidelines
PALTmed Guidelines, often distributed as detailed PDF resources, echo the concerns regarding the sole use of sliding scale insulin, advocating for a more structured approach to inpatient diabetes management.
These guidelines emphasize that relying solely on sliding scale doesn’t address the underlying physiological issues causing hyperglycemia and can lead to unpredictable glucose fluctuations.
PDF documents from PALTmed promote the implementation of basal-bolus insulin regimens, coupled with regular glucose monitoring, as the preferred method for achieving glycemic control in hospitalized patients.
PALTmed’s recommendations, available in PDF format, stress the importance of transitioning patients to scheduled insulin as quickly as possible, minimizing the duration of sliding scale use.
The guidelines also address the need for clear protocols and staff education to ensure consistent and safe insulin administration, downloadable as a comprehensive PDF resource.
Choosing Wisely Recommendations
Choosing Wisely, a campaign promoting appropriate medical care, strongly advises against the routine use of sliding scale insulin as a standalone treatment for hyperglycemia, often summarized in accessible PDF guides.
Their recommendations, frequently available as a downloadable PDF, highlight that sliding scale doesn’t address the root causes of elevated blood sugar and can contribute to inconsistent glucose control.
PDF resources from Choosing Wisely advocate for a shift towards scheduled insulin regimens, emphasizing the importance of individualized treatment plans based on patient needs and preferences.
These recommendations, presented in concise PDF formats, encourage healthcare providers to prioritize basal-bolus therapy or continuous insulin infusion over reactive sliding scale adjustments.
Choosing Wisely’s PDF materials underscore the need for careful assessment and management of diabetes in hospitalized patients, moving away from practices with limited evidence of benefit.

Potential Risks and Complications
Sliding scale insulin, detailed in PDF protocols, carries risks of hypoglycemia and hyperglycemia due to reactive dosing; inconsistent control is common.
PDF guides often warn about the potential for wide glucose fluctuations, necessitating frequent monitoring and careful adjustments to the insulin scale;
Hypoglycemia
Sliding scale insulin protocols, often presented as PDF documents, inherently increase the risk of hypoglycemia due to their reactive nature. Because dosages are adjusted after blood glucose measurements, there’s a potential for overcorrection, especially if meals are delayed or insufficient.
PDF-based protocols should clearly outline hypoglycemia management procedures, including the administration of rapid-acting glucose and repeat blood glucose checks. These documents frequently emphasize the importance of recognizing early symptoms – shakiness, sweating, confusion – and prompt intervention.
Furthermore, PDF guides should detail specific thresholds for intervention, such as treating blood glucose levels below 70 mg/dL. Consistent monitoring, as highlighted in these resources, is crucial to prevent severe hypoglycemic events, particularly in vulnerable populations.
Careful review of the sliding scale PDF by healthcare professionals and patients is essential to minimize this risk.
Hyperglycemia
Sliding scale insulin PDF protocols, while aiming to correct high blood sugar, can sometimes contribute to persistent hyperglycemia if not implemented correctly. The reactive nature of these scales means they address glucose elevations after they occur, potentially leading to a cycle of correction and rebound.
PDF guides should clearly define the upper limits of the sliding scale and outline procedures for managing blood glucose levels that remain consistently high despite dosage adjustments. These resources often recommend contacting a physician for further evaluation and potential changes to the overall diabetes management plan.
Furthermore, PDF documents should emphasize the importance of identifying and addressing underlying causes of hyperglycemia, such as dietary indiscretions or illness. Consistent monitoring, as detailed in these guides, is vital to prevent chronic hyperglycemia and its associated complications.
Effective use of the sliding scale, as outlined in the PDF, requires diligent assessment and proactive intervention.
Inconsistent Glucose Control
Sliding scale insulin PDF protocols are frequently criticized for promoting inconsistent glucose control due to their reactive, rather than proactive, approach. These PDF guides often lack detailed instructions on addressing the root causes of fluctuating blood sugar, leading to a cycle of chasing numbers.
A key concern highlighted in many PDF resources is the potential for wide swings between hyperglycemia and hypoglycemia. The sliding scale adjusts insulin based on current readings, without accounting for factors like meal timing or activity levels, contributing to instability.
PDF documents should emphasize that sliding scale is generally a temporary measure, not a long-term solution; They should advocate for transitioning to more comprehensive regimens, like basal-bolus therapy, to achieve consistent glycemic control and minimize complications.
Ultimately, consistent glucose control requires a personalized, proactive plan, not solely reliance on a reactive sliding scale.

Recent Research and Developments (2025)
2025 research evaluated sliding scale regular human insulin (RHI) algorithms, documented in PDFs, to identify patients at risk for severe hyperglycemia.
Studies suggest that PDF-based protocols need refinement for optimal patient outcomes and to address inherent limitations of this approach.
Evaluation of Different Sliding Scale Algorithms
Recent evaluations, often detailed in PDF reports, have focused on comparing the efficacy of various sliding scale insulin (SSI) algorithms. A retrospective 2025 study analyzed two RHI (regular human insulin) SSI algorithms, aiming to pinpoint patients prone to developing severe hyperglycemia while utilizing these protocols.
These PDF-based analyses highlight the inconsistencies inherent in SSI, demonstrating that certain algorithms may not adequately prevent extreme glucose fluctuations. Researchers are investigating whether modifications to existing algorithms, or the development of entirely new ones, can improve glycemic control.
Furthermore, the accessibility of these algorithms in PDF format allows for wider dissemination and scrutiny within the medical community, fostering a collaborative approach to optimizing insulin delivery strategies. The goal is to minimize risks associated with SSI and enhance patient safety.
Use of Second-Generation Basal Insulins (Glargine-300, Degludec)
Current guidelines, often summarized in accessible PDF documents, suggest considering second-generation basal insulins – glargine-300 and degludec – as alternatives to traditional methods, including sliding scale insulin. These newer insulins offer flatter, more consistent action profiles, potentially leading to improved glycemic control and reduced hypoglycemic risk.
PDF resources from organizations like the ADA emphasize that basal insulins are generally preferred over SSI for inpatient diabetes management. While SSI may still be used in specific situations, the integration of glargine-300 or degludec can simplify regimens.
Information available in PDF format details how these insulins can be incorporated into comprehensive diabetes protocols, moving away from reactive sliding scales towards proactive, basal-driven approaches.